Inherent biases and limitations of the NPS approach are uncovered during my time at Forum Business Research, lending data-driven support to the novel feedback technique – Patient Smile®
Brief
In this PX research project, I delved into the nuances of healthcare feedback systems, specifically the Net Promoter Score (NPS®) survey, and its impact on patient experiences. Through extensive research and data analysis, I uncovered the inherent biases and limitations of the NPS approach.
Result
Lead to the development of a novel feedback technique – Patient Smile®. This innovative solution aims to capture genuine, emotion-rich patient stories, fostering a patient-centric culture and driving positive transformations within healthcare organizations.
This is a research project where I wore the following hats:
Qualitative Research | User interviews, contextual inquiry, observation studies
Data Analysis | Excel, R
Visualization + Wireframing | Figma
Timeline | May '22 - May '23
Team | 2 PX researchers, 1 PM
Despite consistent efforts to improve the patient experience (PX), multiple hospitals across India were failing to increase a trusting patient base that would recommend their business.
Well-established, multi-speciality hospitals in various major cities in India faced the same challenge with improving patient experience.
Happy patients make for promoters of the hospital by recommending the hospital to friends and family. Thus hospitals directed significant resources into keeping their patients happy. However, despite relying on traditional and credible methods like the Healthcare Net Promoter Score (NPS®), something was amiss.
Google reviews kept dipping. Patients were not giving referrals. Patient experience management was failing.
To understand the problem we first looked at the correlation between the NPS analytics and the Google reviews of two hospitals.

Numbers in a spreadsheet reveal valuable insights no doubt, but that story is always incomplete. And that's why we investigated the patient feedback systems in-person at both hospitals.
Changes to an expected experience may inadvertently create usability hurdles, leading to confusion, reduced productivity, and user frustration. And assessing the impact of these changes will ensure a smooth transition to the updated experience.
Conducting semi-structured interviews with patients, hospital staff, and healthcare professionals to gather their perspectives, experiences, and feedback on the existing NPS survey process.
Observing patients in their natural environments, such as hospital waiting rooms and during their interactions with healthcare providers, to gain insights into their behavior, emotions, and pain points.
Examining relevant literature from cognitive psychology, user experience, and healthcare domains to understand the theoretical foundations and best practices related to patient feedback and experience.
Our multi-pronged research approach uncovered inherent qualities of the NPS survey design that shed light on the PX trends we see across both hospitals.
The classic NPS survey is short in order to serve the purpose of brevity. The reasoning: patients don’t have much time to spare for feedback.
After all, patients are not here to make hospitals better, they are here to get the right treatment. This is an assumption. We have evidence to show that in some cases, this assumption about patients’ is detrimentally wrong.
Questions that are designed in a quantitative form automatically activate the rational reasoning in patients.
Patients, when presented with a 0 - 10 scale to rate on, start with the default of 10 being perfect, impeccable service. They then try to reason their way to score lower. Patients thus try and recall reasons to justify scoring lower, following the faulty prompting by the survey design.
The NPS survey is designed to draw the patients’ focus to issues they faced.
Questions are crafted such that patients remember their negative experiences at the hospital. While a part of the feedback is intended to shed light on the hospital’s problem areas, it is only a part.
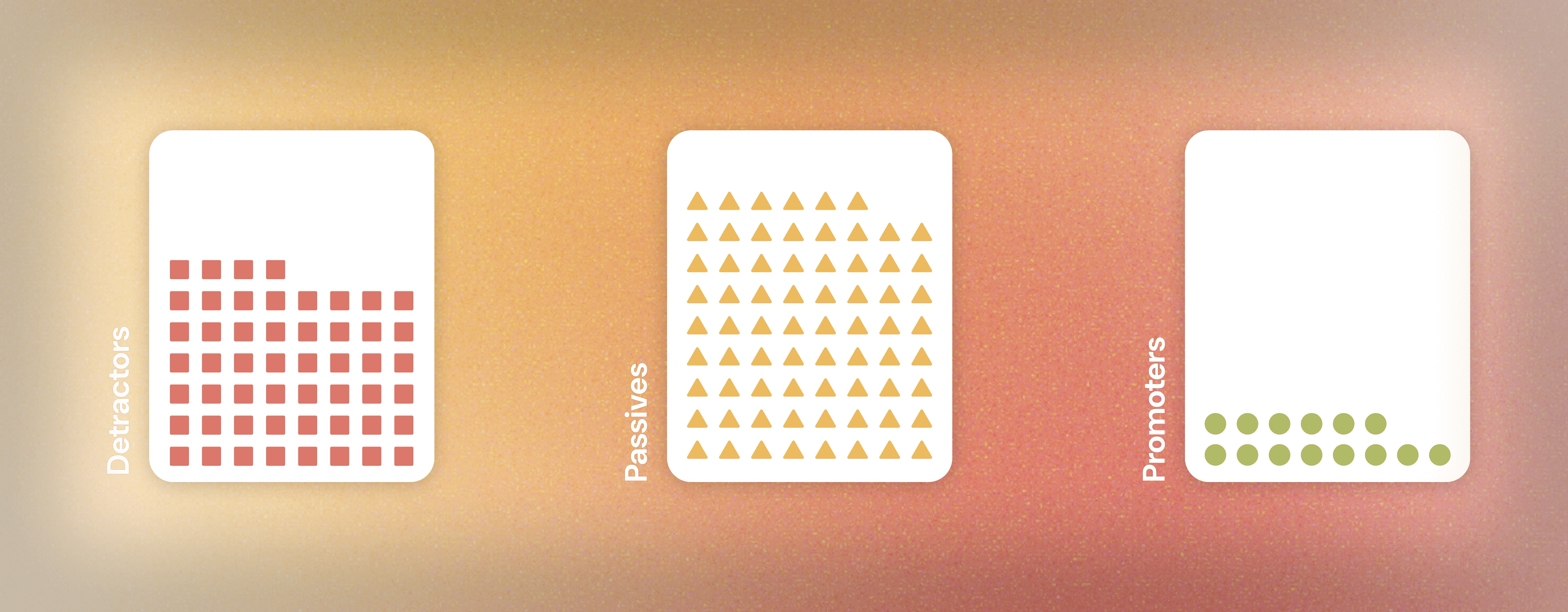
Feedback obtained through the NPS survey reflects a distorted ratio of +ve and -ve experiences. While the surveys might bring attention to the weak points in the patients’ journey, they do not report on the good moments of their journey.
We are more likely to remember negative experiences over positive experiences. Negative emotions generally involve more thinking, and the information is more thoroughly processed than positive ones.
This has to do with the additional recruitment of sensory processes during the encoding of negative items that allow negative items to be vividly remembered.
And hence, -ve events are stored in memory for longer durations with easier, faster retrieval on cue.
The framing effect is when our decisions are influenced by the way information is presented.
Because of the way NPS questions are worded, they have an automatic framing effect that restricts the scope of patients’ feedback to areas of improvements. This causes them to focus information retrieval on moments of disappointment intheir journey at the hospital.
Our choices are impacted by the way options are framed through different wordings, reference points, and emphasis.
Our user interviews with both the healthcare staff and the patients revealed a two-fold detrimental effect.
We begin by collating and analyzing the insights picked up from various stakeholders and research methods. Next, we craft our How Might We's which forms a framework for our Behavioral Science team to design a novel feedback solution using.
This work ultimately results in Patient Smile®.
HMW design a feedback system that mitigates the negativity bias and encourages patients to recall and share positive experiences as well?
HMW frame feedback questions to elicit more balanced and holistic responses from patients, capturing both positive and negative aspects of their experiences?
HMW create a feedback environment that makes patients feel heard, valued, and empowered to share their stories and emotions freely?
HMW present feedback data to healthcare providers in a way that celebrates successes, boosts morale, and motivates continuous improvement?
Patient Smile employs a novel feedback technique that corrects the bias caused by the NPS design.
The feedback technique is designed to first elicit in the patients the emotions associated with the patient experience journey, followed by a rationalization of evoked emotional impressions by using metaphors as a crutch.
This is done to circumvent the framing effect and the possibility of priming the patient.
We recognize that patients are not like any other customers. They are vulnerable, often scared and helpless.
Our novel feedback technique is designed to make the patients feel heard. The approach is designed to actually hear their stories, map their emotions at multiple touch points during their journey in the hospital, and address their concerns, if any, before they leave the hospital. Not a single patient leaves the hospital feeling ignored, overlooked, or unseen.
The technique is designed to evoke emotions associated with the patient's journey first, followed by a rationalization of these impressions using metaphors as a guide.
We analyzed the output that Patient Smile generated in the two hospitals 3 and then 6 months later. We compared this data with data that NPS generated.